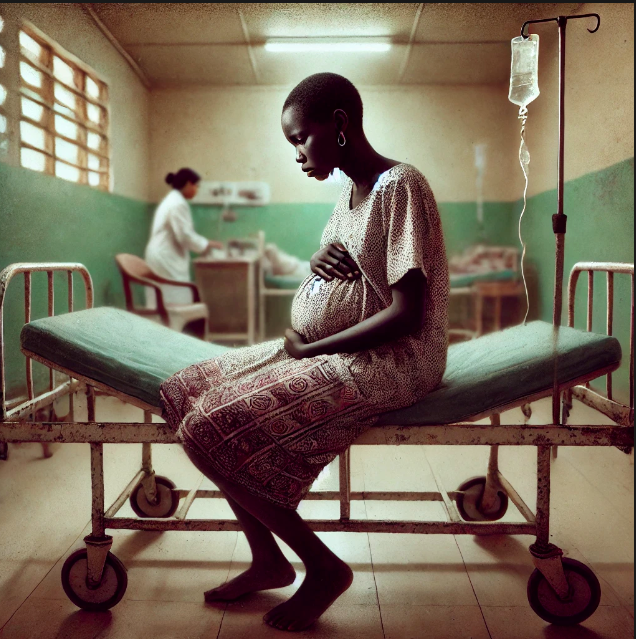
 The study reveals many maternity wards have become death
traps.
The study reveals many maternity wards have become death
traps.Every year, thousands of expectant women in Kenya seek refuge in health facilities to give birth safely.
But
some of them do not survive.
An analysis of the deaths of 1, 162 women in 2021 reveals how and where they died.
The analysis reveals that Nairobi, Kisumu and Mombasa cities are among the ten counties whose hospitals recorded the highest proportion of these deaths. These counties exceed 125 maternal deaths per 100,000 live births.
They are Tana River, Mandera, Machakos, Kilifi, Taita Taveta, Kisumu, Nairobi, Garissa, Mombasa and Isiolo.
The ten with the lowest deaths, below 75 per 100,000 live births, are Baringo, Siaya, Nyamira, Elgeyo-Marakwet, West Pokot, Nandi, Kiambu, Laikipia, Nyeri, Samburu, and Marsabit.
The analysis was done by researchers from the University of Nairobi and University of Birmingham, led by Dr Francis G. Muriithi, of Birmingham.
“There is evidence of sub-national variability in Kenya’s iMMRs (institutional maternal mortality ratios) at regional and county levels and between various health facility levels in the referral system,” Dr Muriithi and his colleagues said.
“Understanding these reasons is crucial for developing alternative and targeted strategies for improving maternal health outcomes.”
Their study, published in Frontiers in Global Women’s Health, is based on 2021 health facility data from the District Health Information System (DHIS-2), a portal where all health facilities in Kenya report their data.
The study is titled: “An exploration of sub-national variability in institutional maternal mortality ratios in Kenya.”
The 2022 Kenya Demographic and Health Survey (KDHS) indicates that nearly 90 per cent of women in Kenya give birth under the care of skilled health professionals.
This should mean fewer deaths. But the study reveals many maternity wards have become death traps.
That is because they lack proper resources– such as medical supplies, trained staff, and a functioning referral system.
Dr Muriithi and his colleagues also examined maternal deaths at different levels of healthcare facilities, from local clinics to national referral hospitals.
They found that Level 6 hospitals – national referral facilities –had the highest iMMRs at 683 per 100,000 live births. Level 2 facilities, which include small clinics and dispensaries, also showed high iMMRs of 407 per 100,000 live births, suggesting that lower-level facilities might lack the resources to handle obstetric emergencies.
“The referral system plays a crucial role in
maternal survival,” they explained. “Level 6 hospitals receive the most critical
cases, which may explain their high iMMR. However, improving the capabilities
of lower-level facilities could reduce the burden on referral hospitals and
improve overall outcomes.”
Kenya’s health facilities are categorised into six levels: Level 1 (community health services), Level 2 (clinics and dispensaries), Level 3 (health centres and nursing homes), Level 4 (county hospitals), Level 5 (county referral hospitals), and Level 6 (national referral hospitals).
The leading causes of maternal deaths in Kenya were obstetric hemorrhage (39.7 per cent), hypertensive disorders (15.3 per cent), and non-obstetric complications (19.8 per cent). Additionally, healthcare worker-related factors were frequently cited, including delays in starting treatment, inadequate monitoring, and insufficient clinical skills.
“Healthcare worker-related factors accounted for a significant proportion of maternal deaths,” the authors said. “Delays in initiating treatment were recorded in 32.9 per cent of cases, while inadequate monitoring contributed to 26.9 per cent of maternal deaths.”
They also pointed to systemic issues such as inequitable healthcare access, variations in political commitment to maternal health, and disparities in the availability of life-saving resources like blood transfusions and emergency medications.
The researchers emphasised that addressing these factors could significantly reduce maternal mortality rates.
One of their key recommendations is to adopt an asset-based approach, often referred to as the “positive deviance” model. This approach involves studying regions and healthcare facilities with lower-than-average maternal mortality rates to identify and replicate successful practices.
“If positively deviant behaviors and practices are
identified, they could form the basis for improving maternal healthcare
delivery processes nationwide,” the researchers suggested.
In Africa Seychelles has the lowest IMMR of three, according to the WHO.