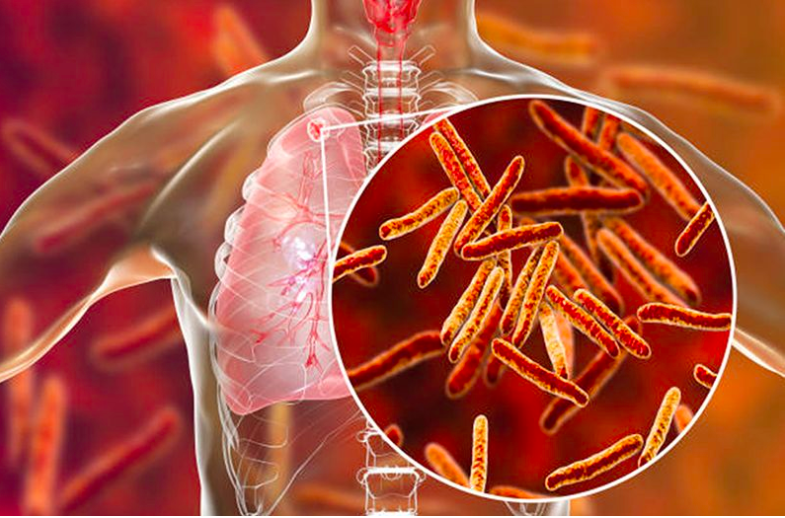
According to the World Health
Organisation (WHO), a total of 1.3 million people died from Tuberculosis (TB)
in 2022, including 167, 000 people living with HIV.
TB is not only the oldest infection
known to man but is also the most fatal single agent infection globally. Even
at the height of the Covid pandemic, TB was the second leading cause of death
from a single infectious agent, with nearly 2.5 million people falling ill and
424 000 lives lost in 2022. Although
TB affects all organs, 80 per cent of
the disease affects the lungs and it is thus readily transmissible to others
via droplets coughed up. This way, up to a quarter of the entire global
population has been infected with tuberculosis and carry a ten percent risk of
developing tuberculosis as a disease in their lifetime.
Although our rate of detecting TB
disease has been low with a failure to pick up to 40 per cent of disease in the
recent past, Africa has seen a significant increase between 2020 and 2022,
rising from 60 per cent to 70 per cent of cases being detected, according to the
2023 WHO Global Tuberculosis Report.
This year’s theme for World TB Day is
“Yes! We Can End TB: Commit, Invest, Deliver,” which offers an opportunity to
reflect on the ongoing efforts and encourage stronger commitment at local,
national and international levels to end TB, including by combatting the
growing threat of drug-resistant TB.
The risk of infection from
tuberculosis and the risk of developing the disease are driven by many health,
lifestyle, socio-economic and environmental factors. Certain medical conditions
can increase a person’s risk for TB disease such as tobacco use, HIV caused by
weakened immune system, diabetes, being malnourished and harmful use of
alcohol.
Despite medical advancements, TB still
devastates millions globally, with far-reaching health, social and economic
consequences. The Sub-Saharan region, which bears a significant burden of the
disease, must implement a combination of strategies to end the TB epidemic by
2030.
Utmost, efforts should be made to
expand access to diagnosis and the treatments of TB. We must strive to bring TB
services closer to the communities, especially the rural areas, who have always
been left behind towards the diagnosis and treatment of TB. This should be implemented
through offering primary healthcare services to ensure early and accurate
detection of TB, marking a crucial step towards ending the TB epidemic. Without
treatment, 50 per cent of tuberculosis patients will die and untreated TB
increases the pool of infectious humans to compound the public health problem.
Even with cure, many survivors have residual diseases in their lungs with
long-term health concerns that together account for nearly half of the
disability caused by TB.
Secondly, drug-resistant TB is a
significant contributor to the disease burden, to the cost of healthcare and
compounds the public health problems of tuberculosis by several factors. Tackling
drug resistant TB should be implemented by strengthening TB surveillance
systems to detect and monitor drug-resistant cases. This can be achieved by
ensuring uninterrupted TB drug supply by the Government to prevent shortages of
essential TB drugs and by expanding access to new and more effective drug
regiments.
Thirdly, integrating TB services with other
healthcare programs can be an effective strategy towards tackling TB epidemic. For
example, the high prevalence of HIV in Sub-Saharan region worsens the TB
problem, as HIV weakens the immune system, making individuals more vulnerable
to TB. According to the WHO, people who are infected with HIV are 20 to 30
times more likely to develop active TB. Therefore, efforts should be made to
integrate TB screening and treatment services within the HIV programmes. In
addition, maternal and child health services should be incorporated where pregnant women and children should be prioritised for TB
preventive and routine screening.
Further,
we should strengthen community engagement and innovative health promotion
programs including leveraging social media platforms. The myths and
misconceptions around TB need to be addressed through community-driven
education programs via mainstream media, formal structured campaigns and
strategic advertising. Engaging local leaders and religious leaders as TB
champions in raising awareness and promoting TB campaigns can go a long way
towards achieving this goal.
Finally,
governments must prioritise TB financing through national budgets provision instead
of relying heavily on external donors. A recent example is the withdrawal of
USAID funding, which has severely interrupted progress in TB programmes. This
situation underlines the need for governments to demonstrate commitment by
filling the funding gap. Without domestic resource mobilization, there is a
real risk of losing momentum in the fight to end the TB epidemic.
It
is crucial to recognise that ending TB demands sustained investment and
innovative approaches to the diagnosis, treatment, and prevention of TB. Through
strong strategic interventions and investments in sustainable TB programmes the
region can play its role towards ending TB epidemic by 2030.
Dr Jumaa Bwika is a consultant physician and assistant professor, head of pulmonology, department of medicine, Aga Khan University Medical College, East Africa.