Can Kenya Achieve population immunity?
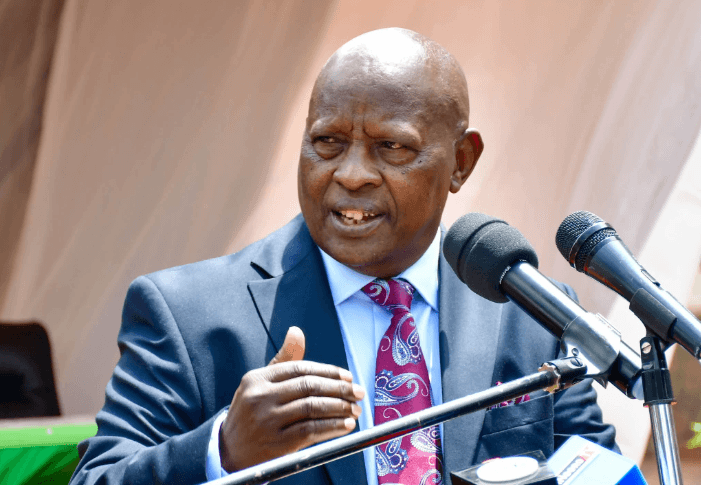
With less than 30% of Kenyans immunised against the COVID-19 virus, is it likely that the country will reach ‘herd or population immunity’ by the end of the year as Health Minister Mutahi Kagwe stated when launching the rapid results vaccination campaign on February 3? During the campaign,the government hopes to vaccinate 10 million Kenyans in a ten day period which translates to one million people vaccinated every day with the goal of increasing the number of those fully vaccinated to 23 million.
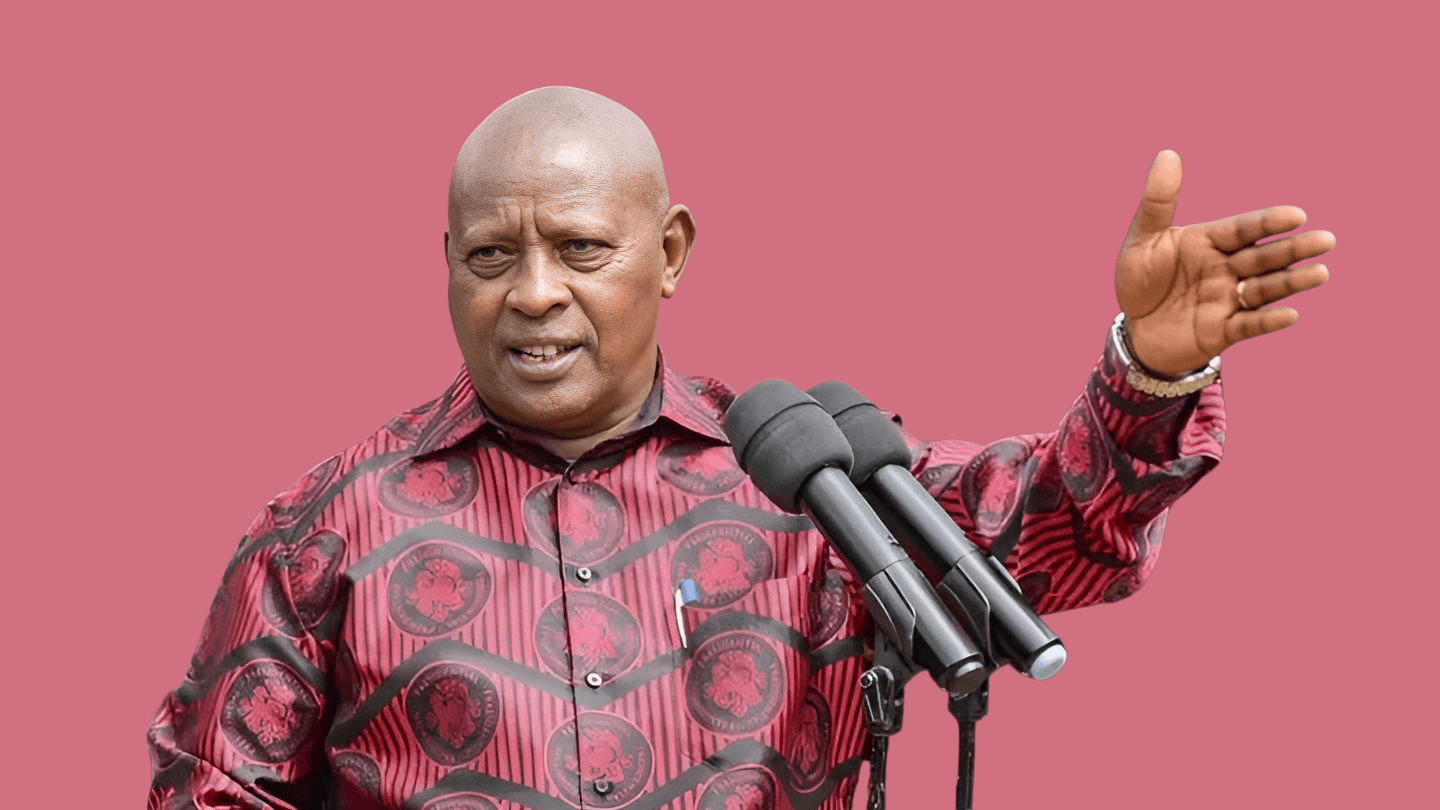
The initiative launched in collaboration with Interior Cabinet Secretary Fred Matiangi will see at least 10 million Kenyans receive a COVID-19 vaccine. The ultimate goal, the two ministers said, was to have at least 70 per cent of the country's population vaccinated.
"The goal of the drive is to create a strong herd immunity against COVID-19 and its variants," Matiangi said.
Acting Health Director-General Dr. Patrick Amoth has stated in various interviews that if 70% of the population get fully vaccinated, the county will achieve population herd immunity by the end of 2022, providing some immunity to the Covid-19 virus and slowing its spread.
What you need to know about Population Immunity https://t.co/f2strlOQmu pic.twitter.com/uil1k23v58
— TheStarKenya (@TheStarKenya) March 1, 2022
He explains that herd immunity will be determined by the evolutionary changes in the coronavirus, citizens following existing preventive measures and at least 70% of the population getting the COVID-19 vaccine.
In order for this to happen, the government needed to ensure long-term availability and citizens access to more and different Covid-19 vaccines.
So, what exactly is population immunity, how do we achieve it, and what factors will indicate we have achieved it?
What is population immunity?
This is defined as the point at which community spread of an infectious disease stops or slows because the majority of the population has developed immunity to the disease through prior infection and or vaccination. Unvaccinated and/ or immuno-compromised individuals will thus be surrounded by a ‘herd’ of people who are immune. This breaks the chain of infection, reducing the transmission rate thus slowing the spread of the disease.
Instances throughout history where population immunity was achieved.
Measles, Smallpox and Polio are examples of infectious diseases that were once widespread but are now uncommon in most parts of the world as a result of vaccines. Smallpox was the first ever human disease successfully eradicated through widespread vaccination campaigns, It was also the first vaccine-preventable disease, with the World Health Organisation certifying the global eradication of smallpox on 9 December 1979, and the WHO General General Assembly endorsing and recognizing the total eradication of Smallpox on 8 May 1980.
We occasionally see outbreaks of vaccine-preventable diseases in communities with lower vaccine coverage because they lack herd immunity. (An example is the 2018 measles outbreak in Nairobi county's Kamukunji sub-county.)
What factors have an impact on population immunity?
This is a numbers game influenced by other variables such as the pathogen's transmissibility, vaccine efficacy and the behaviour and immunological characteristics of the population in which the pathogen (virus) is spreading.
Covid-19 became a pandemic because of its high virulence— the ability of a virus to infect and cause disease. If a virus is easily transmissible and the population is densely packed and mobile, a large proportion of the population will require immunity (via vaccination) to stop the spread of the virus, whereas if the virus is less transmissible or the population is not as mobile, fewer people will require immunity to slow the spread of the virus.
In either case, the population herd immunity threshold will be different.Reaching a herd-immunity threshold is also likely to be difficult due to factors such as vaccine hesitancy, the emergence of new variants, access to adequate vaccines, and the delayed arrival of vaccinations for children.Scientists have been forced to reconsider their previous assumptions about herd immunity as a result of new developments that have happened such as the mutation of the virus and the emergence of new variants which are more transmissible e.g. the delta and omicron variants. Reaching herd immunity is now regarded more as an aspiration rather than actual goal.
The emergence of new COVID-19 variants may have an impact on the herd immunity threshold in the population. The WHO estimated population immunity threshold to be at 60-70 percent of the total population at the state of the pandemic, when dealing with the original Sars-CoV-2 strain. But with the emergence of new and more transmissible variants like Delta and Omicron, the threshold is likely to be revised upward to 80 percent, assuming that everyone is vaccinated or previously protected. Preliminary data about omicron and vaccines is rapidly becoming available, revealing lower vaccine effectiveness. Vaccines are thought to be 30%-40% effective at preventing infections and 70% effective at preventing severe disease, according to best estimates.
Since the beginning of the pandemic, we have a lack of adherence to behavioural changes such as mask wearing, social distancing, and sanitising which were intended to slow the spread of the virus. There are also social inequalities, such as populations living in overcrowded housing without access to clean running water, masks, or soap.
“If these interventions are not followed, virus transmission will continue to accelerate. This will raise the population immunity threshold compared to the 60-70 % threshold set when the population was more cautious,” explains this report by the European Medicines Agency.
Breakthrough infections, in which people who have been fully vaccinated become infected, are also a major concern when attempting to achieve population herd immunity. The Delta and Omicron variants are highly infectious and transmissible, and they have the ability to evade immunity even in populations with high vaccination rates.
Vaccine effectiveness refers to how well vaccines perform in the real world. Efficacy (performance in clinical trials) of available vaccines ranges between 70% and 95%, but performance in real-world conditions is likely to be lower, and other factors such as vaccine transportation and storage can reduce vaccine effectiveness.
The vaccines’ ability to provide long term protection will also have an impact on the achievement of herd immunity. While the current vaccine responses are expected to last for at least six to nine months this does not mean that they will protect people against infection from variants that are evolving. The vaccines, on the other hand, aid in preventing severe infections of COVID-19.
Another critical factor that must be considered is mass vaccination. Earlier expert estimates stated that 70 percent of the total population needs to be vaccinated in order to achieve population immunity. “In the face of an evolving and increasingly transmissible virus, high population immunity is required to achieve this goal, which means vaccinating broadly. Based on current knowledge, this requires fully vaccinating at least 70% of the world’s population, accounting for most adults and adolescents and for the vast majority of those at risk of serious disease,” according to the WHO global vaccine strategy.
Experts predict that meeting this goal will be difficult. Significant efforts and investments have been made to secure the necessary vaccine supplies, while also addressing issues with vaccine acceptance and gaps in countries' capacity to deliver the doses.
As of February 28, Kenya had fully vaccinated 7,575,103 people representing 27.8% percent of adults who are fully vaccinated. This is far below what is required to achieve population immunity. However, Dr Willis Akwale, the Health Ministry’s COVID-19 task force chairman is optimistic that the country will be able to vaccinate 19 million adults (which is 70% of the adult population) by end of June this year and has set a target of vaccinating the entire adult population of 27 million by the end of the year. Increasing vaccination posts from 200 to 3,000 and introducing innovative ways to get to hard-to-reach communities, extending vaccination centre hours are among some of the strategies that the government has adopted to increase vaccine uptake.
One impediment has been a lack of supply. Vaccine shipments through the global Covax donation program began in Kenya in March 2021, but the doses delivered represented only a small portion of what is required. In addition to widespread mistrust in government, misinformation, and disinformation, vaccine hesitancy has been a barrier to Covid-19 vaccinations, despite the fact that childhood vaccinations are widely accepted.In response to the supply issues, health minister Mutahi Kagwe announced in December last year that the country would begin producing COVID-19 vaccines by April 2022. So far, the government has allocated Sh2.5 billion for the establishment of the new Kenya Biovax Institute which is being put up in collaboration with KEMRI.The vaccine production plant which will be located at Embakasi, will help address the vulnerability Kenya has to deal with future health emergencies.
County governments have come up with some innovative ways to inform, educate, and get people to take the vaccine in order to raise awareness and drive uptake of the vaccines. The Pastoralist Information Network, based in Isiolo, Kenya, initiated a program in which they are offering COVID-19 shots to people as well as various vaccines for camels in the border regions of Kenya and Ethiopia.
In addition, the government has worked with religious organisations and other partners to ensure that churches and other places of worship are used as vaccination sites during the week when they are not being used for religious services.
In Northern Kenya , women groups have been conducting house-to-house campaigns to debunk vaccine myths that have been circulating in their communities and to encourage people to get the vaccine. To raise awareness about the vaccine, community radio stations have also broadcast public health information.
Nelson Muriu, the county director of health services in Nyeri, told an international conference that since the curfew was lifted, the county government has extended the hours during which people can get their shots. As a result, people can now get vaccines in the evenings and at night.
Are there countries that have achieved 70% vaccine coverage?
The majority of African countries have yet to achieve 70 percent vaccine coverage. This is due to 'vaccine apartheid,' a term that is increasingly being used to describe the gap in vaccine access between the world's richest and poorest countries.
Winnie Byanyima, the executive director of UNAids and a UN undersecretary general, warned in an op-ed published in the Guardian newspaper a year ago: "We are witnessing vaccine apartheid that is only serving the interests of powerful and profitable pharmaceutical corporations while costing us the quickest and least harmful route out of this crisis."
Vaccine apartheid has resulted in significant doses of vaccines being denied to people living in many countries in the Global South. According to some reports, "133 doses of COVID-19 vaccine have been administered for every 100 people in high-income countries, while only 4 doses have been administered for every 100 people in low-income countries."
Reaching the herd immunity threshold any time soon will necessitate a more robust rollout of vaccine programs in all countries. This entails addressing the issue of inequitable vaccine distribution around the world, as well as increasing vaccine uptake by making vaccines available to the entire global population. "Unless we reach the same sort of threshold around the same time," says Dr EricOsoro “we may not be able to achieve population immunity."
And is it really true that having a large % of the population vaccinated will stop covid spread? Many experts are quick to dismiss the concept of herd immunity as it creates the illusion that we will eventually be able to eradicate this virus. That is highly unlikely to occur. According to these experts, the coronavirus will continue to circulate even if 70% of the population is immunised.
They warn of the dangers of continuing to make people believe it is possible to achieve herd immunity, which may contribute to people losing faith in vaccines.
What is the percentage of people who must be immune to COVID-19 in order for herd immunity to be achieved?
According to a summary of the WHO’s 2022 vaccination strategy, the global community should aim to vaccinate 70% of the world’s population against COVID-19 by mid-2022. The goal is to “substantially increase population immunity” in order to protect people worldwide from disease, protect the health system, fully restart economies, restore the health of society, and reduce the risk of new variants. The WHO warns that due to lack of adequate vaccines, the world is not ready to end the pandemic .
Scientists are still learning about immunity to COVID-19. Most people who are infected with COVID-19 develop an immune response within the first few weeks, but we don’t know how long or strong that immunity lasts, or how it differs between people. There have also been reports of people getting infected with COVID-19 a second time.
We won't be able to predict the COVID-19 immunity until we better understand how much of a population is immune and how long that immunity lasts for. “As more and more people get vaccinated, the rate of transmission of the virus is reduced. Kenyans must be vaccinated in order for the SARS-CoV-2 virus to be like one of the numerous other viruses that circulate and cause mild respiratory illness or less frequently, severe disease,” says Dr. Eric Osoro.
This article was produced by the Africa Women’s Journalism Project (AWJP) in partnership with Article 19, Meedan and the International Center for Journalists (ICFJ).
WATCH: The latest videos from the Star