The Covid-19 vaccine rollout continues to be ramped up in Kenya through donations or through accessing the vital doses from Covax, the UN-backed partnership between the World Health Organisation, the Gavi vaccine alliance and the Coalition for Epidemic Preparedness Innovations.
Covax has been sending vaccines to developing countries, funded by high-income countries and international organisations like the Bill and Melinda Gates Foundation.
Kenya has so far administered about 8.3 million doses of Covid-19 vaccines. In the last week, nearly 88,000 doses per day have been administered, which is the fastest seven-day pace it has achieved so far. The country has so far received more than 23 million doses of Oxford/Astrazeneca, Moderna, Johnson & Johnson, Pfizer and Sinopharm.
In an attempt to boost the vaccination rate, Health CS Mutahi Kagwe issued a directive warning Kenyans they would be barred from bars, restaurants and public transport unless they produced evidence they had been vaccinated.
The directive was intended to boost and reach the Ministry of Health’s target of vaccinating 10 million by the end of this month. On Tuesday December 15, the court dismissed this directive as unconstitutional.
There are 16 vaccines authorised in early or limited use (emergency use) and nine approved for full use in the world, with 43 in phase 3 (last phase) of clinical trials, which involve large-scale efficacy tests.
In Kenya, six vaccines have been approved for use: Moderna, Pfizer/BioNTech, Sputnik V, Johnson & Johnson (Janssen), Oxford/ AstraZeneca and Sinopharm (Beijing).
Based on the technology used to create the vaccine and how they work, they have been divided into five different categories.
VACCINE TYPES, DIFFERENCES
The first is the whole virus category. There are two different types of whole virus vaccines: live attenuated (weakened) and inactivated.
Live attenuated uses a weakened form of the virus. They are genetically modified in a way that the virus is not able to cause disease but still generates an immune response that protects the body in case of an infection. However, they may not be suitable for people with a compromised immune system. An example of such a vaccine is CoviVac.
With inactivated vaccines, the virus is killed or altered so that they cannot replicate. Thus, they cannot cause disease, against which they protect you from and are, therefore, suitable for those with a compromised system. To ensure ongoing protection, a person may need booster shots. Examples are Sinopham and Sinovac.
The second type is the viral vector. This type of vaccine uses a virus that has been genetically engineered so that it cannot cause disease but produce coronavirus proteins, then it is placed in a modified version of a different virus (virus vector).
When the viral vector gets into your cells, it delivers the genetic material from the Covid virus that gives your cells instructions to make copies of the spike protein. Once displayed on the body cells surface, it triggers the immune system to respond by creating antibodies that will fight the Covid-19 virus if you become infected.
The viral vector vaccines cannot cause infection with Covid-19 virus or the viral vector virus. The genetic material delivered does not become part of your DNA. Examples of viral vector vaccines include Sputnik V, Oxford/AstraZeneca, CanSino and Johnson & Johnson.
Thirdly, there is the protein subunit vaccine. This type uses parts of the virus that best stimulate the immune system, which are harmless fragments of spike proteins. Once the immune system recognises the spike protein, it creates antibodies and defensive white blood cells that will fight the infection in case of infection. Examples are EpiVacCorona and Novavax.
The fourth type is the DNA vaccine. This type uses a synthetic DNA fragment (plasmid) that encodes the spike protein of Covid-19 together with a promoter sequence for turning the gene on. Once the plasmids enter the nuclei of cells, they are converted into mRNA, which travels to the main body of the cell, the cytoplasm, and is translated into the spike protein. The body immune system then mounts a response against the protein and produces antibodies that can clear future infections. The plasmids typically degrade within weeks. Examples include Inovio and ZyCoV-D.
The fifth and final type is RNA. This type of vaccine works by introducing into the body the genetically engineered material called mRNA that contains the instruction to make the spike protein of the coronavirus. After vaccination, the body immune cells are given instructions on how to make the spike protein found on the surface of Covid-19 virus and begin making and displaying them on cell surfaces. This causes the body to create antibodies. If you later become infected with Covid-19 virus, these antibodies will fight the virus.
After delivering instructions, the mRNA is immediately broken down (destroyed). It never enters the nucleus of your cells where your DNA is kept, and also does not carry the full information for our cells to make the SARS-CoV-2 virus and, therefore, cannot cause an infection. Examples include Pfizer, Moderna, Curevac.
EFFICACY AND EFFECTIVENESS
Vaccine efficacy refers to the measure of how much the vaccine lowers the risk of getting sick under ideal conditions like a clinical trial. For instance, those participating in the clinical trials are carefully chosen and given specific instructions to reduce their risks. The vaccines are given at precisely the right time and then monitored closely.
It is measured by how many people who got vaccinated developed the outcome of interest, compared with how many people who got the placebo (dummy vaccine) developed the same outcome. A 70 per cent efficacy means that out of the participants in the trial, those who received the vaccine were at a 70 per cent lowered risk of developing disease compared to those who got the placebo. It does not mean the vaccine has a 30 per cent fail.
Vaccine effectiveness, on the other hand, refers to what happens in the real world, when a vaccine is employed to induce community-wide protection. It is measured by observing how well the vaccines work to protect communities as a whole.
Vaccination is a preventive measure not against getting the virus but developing severe infection from the virus. The protection takes time to build, and people must take all the required dosage to achieve maximum protection.
With this in mind, the precautions in place must be adhered to to protect yourself and others who may not be vaccinated as the vaccine builds up maximum protection, a process that takes two to three weeks after every dose.
Most vaccines are still not part of the Covid-19 Vaccines Global Access (Covax) because some of these vaccines are yet to be approved by the WHO for use because of mixed results from their clinical trials, which were not published for peer review, and also lack of transparency on the results of the clinical trials.
Kenya recorded its first case of the new Covid-19 variant, Omicron, on December 15. CS Kagwe urged Kenyans to get vaccinated as this might protect them against getting severe disease if they contract the virus.
Preliminary evidence indicates Covid-19 vaccines may be less effective against infection and transmission linked to the Omicron coronavirus variant. Although Omicron is more transmissible than Delta, research has suggested that it causes less severe disease.
As scientists find out more about the new variant, getting vaccinated and adopting multi-layered protection measures are still required. These include maintaining physical distance, wearing masks, frequent handwashing, testing and tracing.
This article was produced by the Africa Women’s Journalism Project (AWJP) in partnership with Article 19, Meedan and the International Centre for Journalists (ICFJ).









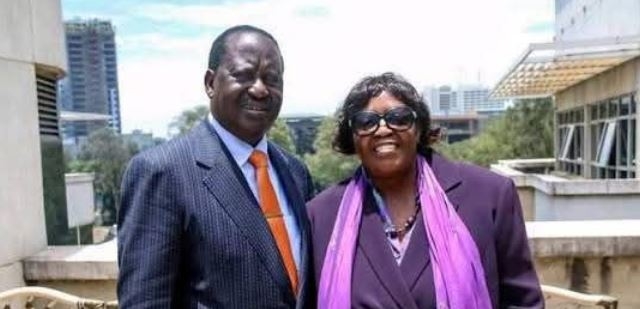


![[PHOTOS] Family, friends receive body of Raila’s sister, Beryl](/_next/image?url=https%3A%2F%2Fcdn.radioafrica.digital%2Fimage%2F2025%2F11%2Fdfe6a9bf-ede1-47a4-bdc0-4f564edb03dd.jpeg&w=3840&q=100)


