Family planning has long been seen as an abomination in the villages of Malindi in Kilifi county.
Especially permanent options, such as vasectomy and bilateral tubal ligation (BTL), which are falsely perceived as libido-killing, cancer-causing surgeries.
Vasectomy remains a hard sell, but women are turning up in droves for BTL after getting more informed.
Many are pulling away from cultural reservations and are streaming into the Malindi Subcounty Hospital to seek family planning services.
The surgeon conducting BTL procedures at the facility is fully booked for the month — about six women are on the waiting list.
“The uptake is snowballing,” says Job Ogutu, a medical officer at the hospital.
“We are not sure if it is about the harsh economy or the rigorous sensitisation programmes we have been conducting in the villages for the past few years.”
For the past more than two years, Kilifi county and Marie Stopes Kenya have been conducting a public sector strengthening campaign to bridge the gap of the unmet needs of contraceptives.
“We experienced pockets of resistance initially. Some people felt that they were being curtailed from getting their preferred family sizes. So, we had to use counter strategies to convince the residents otherwise,” he says.
The campaign is training healthcare workers, equipping health facilities and renovating them to create safe spaces for the administration of post- abortion care and different methods of contraceptives.
Other family planning methods being administered include permanent methods, such as BTL and vasectomy, temporary methods such as injectables and pills, and long-term reversible methods, such as implants and intra uterine contraceptive devices (IUCD).
While the general uptake of contraceptives has gone up, it is the embrace of BTL by women that has taken the campaign by surprise.
I am very healthy today and very comfortable and in fact, if anybody asks me, I will tell him or her that life begins at 50 and after tubal ligation
ENOUGH IS ENOUGH
After two miscarriages and several blood transfusions, Esha Ade, 50, said ‘enough is enough’.
The mother of two underwent the procedure almost two years ago at the Malindi Subcounty Hospital.
“The miscarriages not only affected me physically but also took a toll on my emotional health,” Ade says.
“I remember completely shutting out and almost sinking into depression after the second miscarriage. My husband and I desired to have more children, but after two failed attempts, we decided to go for the permanent method.”
Tubal ligation was mired in myths and misconceptions, but Ade was not daunted.
“I am very healthy today and very comfortable and in fact, if anybody asks me, I will tell him or her that life begins at 50 and after tubal ligation,” she says amid laughter.
Unlike many men, Ade’s husband fully supported her. Having seen her suffer physically and emotionally, not even religion could sway him.
“Islam says if something causes you harm, you should do away with it and everyone could see that the miscarriages were hurting me. I also needed the strength to raise my two children,” Ade says.
After three children, Dorris Welimo outrightly knew she did not want any more children and underwent BTL.
Unlike Ade, the 40-year-old mother of three did not get the full blessings of her husband.
“I had the IUCD inserted after my second child. But later on, I started having baby fevers and had it removed, and that’s when I conceived my third baby. It is at this point that I knew I needed a permanent solution,” she says.
“I only informed my husband of my intentions because after all, it is my body and my choice and four years later, I have no regrets at all. Of course, my husband wishes I did not have it.”
His fears are that Welimo might start cheating since there is no fear of her getting pregnant.
Apart from her husband, Welimo did not tell anybody else of her decision to avoid stigma and ridicule.
All the misconceptions are demystified during counselling. They are also informed that the method is permanent and irreversible and it is 99 per cent effective
COUNSELLED BEFORE SURGERY
Malindi Subcounty Hospital is providing BTL services for free during in-reach programmes courtesy of the public sector strengthening project supported by Marie Stopes Kenya. Walk-ins pay a theatre fee of Sh6,000.
Before undergoing the procedure at the Malindi Subcounty Hospital, one is first taken through a rigorous series of counselling.
“All the misconceptions are demystified during counselling. They are also informed that the method is permanent and irreversible and it is 99 per cent effective,” Ogutu says.
On the day of the surgery, the client is starved and a normal anaesthesia that works around the area of the incision is administered. A small incision is then made, where the fallopian tubes are tied. Recovery only takes three days under heavy pain medication.
Some of the myths attached to tubal ligation are lack of sexual urge, risks of cancer and inconsistent menses, which Ade and Welimo say they have not experienced.
Ogutu says they also faced cultural barriers that require the women to seek permission from their husbands before they make decisions regarding their bodies.
One of the strategies the PSS campaigners used to mitigate the challenges was using trained community health promoters, who would walk from door to door to educate the residents on the different types of contraceptives.
“Most women are also illiterate and are not empowered to confidently make reproductive health decisions,” Ogutu says.
Gynaecologist Dr John Ong’ech says contraceptives are effective for as long as they are used as prescribed.
He says individuals seeking family planning services should visit medical facilities with trained medics and first get counselling.
“The professional, before prescribing family planning, should have your medical history,” Ong’ech says.
“Medical conditions like blood pressure should be made known to the medic before a prescription is given.”
VASECTOMY SHUNNED
While tubal ligation has been embraced by many, vasectomy is still widely avoided.
Since the programme started, only one man in the entire Malindi subcounty has undergone vasectomy.
“We had three men who wanted to have it but two chickened out. One actually walked out on us on the operating table,” Ogutu says.
Even so, the man who successfully underwent the procedure does not want to openly talk about it due to stigma.
A recent survey shows more than half of married men in Kenya are willing to try a new male contraceptive immediately it is available.
The research, titled 'Assessment of demand for male contraceptives: A multi-country study,' says 52 per cent of the men surveyed would use the contraceptives within the first year and only 18 per cent of Kenyan men said they would never use a male contraception.
Reproductive health advocates in Kenya questioned the genuineness of the high interest, noting it is already "very difficult" to get men to support female birth control, let alone a male one.
The Kenya Demographic Health Survey 2022 says Kenya has a 14 per cent unmet need of family planning, down from the 17.5 per cent in 2022.
The survey further says 57 per cent of married women and 59 per cent of sexually active unmarried women aged between 15 and 49 are using modern family planning methods.
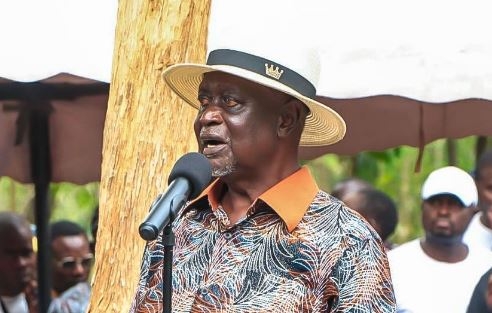
Suba North MP Millie Odhiambo has a bill in Parliament that seeks to empower women to make informed decisions about their reproductive health rights.
The Family Reproductive Healthcare Bill also seeks to work with the Sexual Offences Act to address some of the discrepancies in the law regarding reproductive health rights.
“We must not bury our heads in the sand and start talking about reproductive health rights openly. Women should know that talking about family planning or their menses is not a taboo,” Odhiambo says.
“Access to information regarding reproductive health is critical. Many young people today lack this information, leading to tragic consequences.”
The World Health Organisation says use of contraception prevents pregnancy-related health risks for women, especially for adolescent girls.
When expressed in terms of interbirth intervals, children born within a two-year interval have a 60 per cent increased risk of infant death.
Those born within an interval of three years have a 10 per cent increased risk.
From Ade and Welimo’s testimonies, the reality is that there is still an unmet need of family planning services.
Ogutu says this is due to lack of enough workforce and resources.
“The PSS campaign can only do so much. Many are, however, still unable to raise the Sh6,000 theatre fee as required, and by the time the next in-reach programme takes place, they have either given up or changed their minds or worse, become pregnant,” he says.