Well, this is the story of Jeremy Mathu* (not his real name) from Eastern Kenya.
Born with HIV, Mathu was immediately put on anti-retroviral treatment. He took them religiously and grew up healthy.
At the age of 15, he suddenly became withdrawn and would wear hooded jackets regardless of the hot Eastern weather.
It took a deep probe by Dr Mary Meli, a pharmacovigilance officer attached to the region, to establish that Mathu was growing breasts, which were leaking with milk.
“I dealt with Mathu’s case in 2019. His issue was tricky because this was a teenage boy who was not only going through adolescence but was also experiencing some mysterious developments in his body. The hooded jacket was to protect him from stigma,” she says.
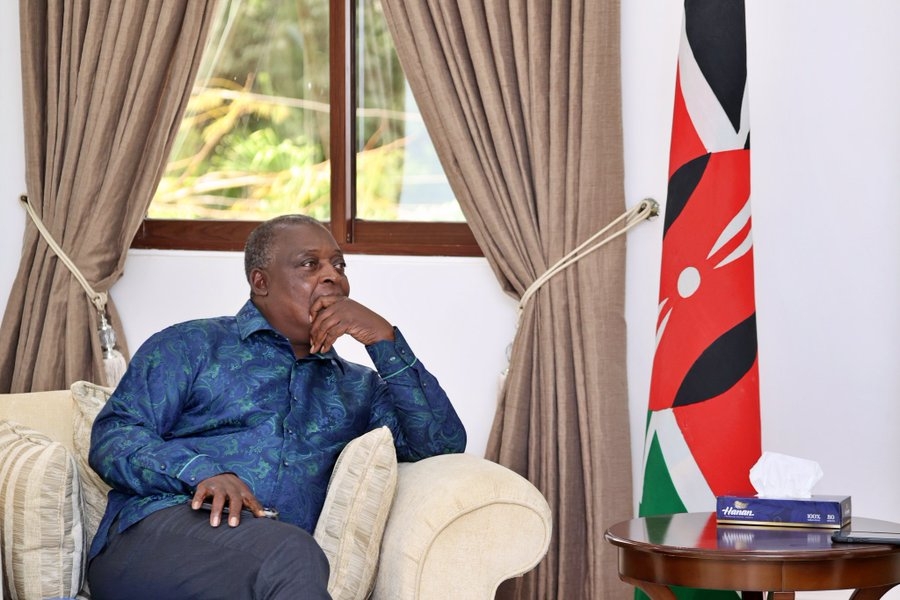
Mary Meli a pharmacovigillance officer at her facility in Nairobi/ CLARET ADHIAMBO
Meli then launched investigations into the specific type of ARV Mathu was taking, which revealed that the drug had quality issues. It had exceeded the required miligrammes.
Investigations revealed that the said anti-retroviral drug had exceeded the required amount of the effervescence molecule, and the side effects of this include CNS (mental illness) and gynecomastia in men, a condition where men grow breasts.
“The drug is supposed to contain 600 miligrammes but whoever formulated it had exceeded the required miligrammes by almost one gramme, making it toxic,” Meli says.
She says the specific company had quality issues and some of their drugs had made many patients to become psychotic.
Dickens Mwamba*, on the other hand, bought some syrup from the streets. He took it for a few days before his skin started decomposing.
Unfortunately after two weeks, Mwamba died.
“His skin turned black, meaning the medicine was killing his skin cells, and eventually his entire body gave in,” Meli says.
PATIENTS EXPOSED
Mwamba and Mathu’s cases are some of the many instances of patients taking substandard medicine Meli has dealt with.
Substandard medicines are medicines with incorrect dosages or wrong active ingredients, leading to ineffective treatments or resistance.
Such products are likely to fuel antimicrobial resistance.
As a pharmacovigilance officer, Meli is tasked with checking the quality of medicines in the market and assessing information about their adverse effects.
She reports all suspicions and the negative effects directly to the Pharmacy and Poisons Board.
“Most of the raids that the board conducts are informed by our reports,” she says.
Jude Mebo* is one of the many patients in Kenya who have fallen victims of substandard medicines.
Mebo says two years ago, he experienced some drug reactions after taking some antibiotics.
“After using the drug for 24 hours, I started having some itches. They turned red and formed watery pimples,” he says.
“The pimples spread very fast, forcing me to rush to the doctor. He asked me to immediately stop taking the medication and then prescribed to me some antihistamine.”
Though recovered, the experience left some physical scars on Mebo’s body.
Last year, PPB conducted around 2,523 inspections in pharmacies.
Of the number, 171 pharmacies were found to be non-compliant.
PPB says the biggest challenge is that most people do not know how to differentiate fake medicine from the legitimate ones.
A research released last year says a fifth of medicines in Africa could be substandard or fake.
The research by Bahir Dar University in Ethiopia analysed 27 studies in the review and found, of the 7,508 medicine samples, 1,639 failed at least one quality test.
Most of these medicines are anti-malarials and antibiotics.
MEDIC’S ACCOUNT
These revelations are supported by June Goro*, a trained medical doctor unable to secure a job due to the rundown employment system in Kenya.
Her quest for a decent life while still practising medicine thrust her into the world of low-income jobs. Last year, one of the low-income jobs she took landed her in a facility in Kibra slum.
“The facility is big. We would see many patients and sell medicines over the counter,” Goro says.
“But after working there for a few days, I noticed some fishy activities. Some people would come from the backdoor and deliver medicines in backpacks.”
Goro’s eyebrows were raised further when the owner of the facility one day took his child for checkup but did not buy the prescribed medicine from the facility.
The medicine invoices were also falsified and the quality of medicines misstated, she says.
“I noticed that they did this to confuse the authorities because there is an invoice system that inspection bodies use to establish if facilities are procuring the right medicines,” the medic says.
“So one day, I gathered courage and spoke to these mysterious suppliers. I lied to him that I wanted to start my own facility and would like the ‘cargo’ to cut on the expenses. He asked me to engage him further but I did not.”
Her conscience would, however, not allow her to continue working at the facility, so she quit.
GLOBAL PROBLEM
Kenya is not the only country grappling with substandard medicines.
Zimbabwe has struggled with the issue for years. So bad is the situation that the medicines are hawked on the streets like sweets.
The country has strict medicine control laws that say persons caught selling counterfeit or unregistered drugs can be sentenced for up to 20 years.
These laws have, however, not helped as impoverished citizens have mastered ways of evading them.
“I sell them because there are no jobs in Zimbabwe and I am trying to earn a living to be able to look after my family. That is how I survive,” one vendor told DW media in a past interview.
In 2019, Uganda’s National Drug Authority, during routine monitoring, discovered substandard and falsified medicines.
The medicines included a broad spectrum of antibiotics used in the management of infections, lower respiratory infection and genital urinary tract infections.
“There’s been a number of reports of substandard cases of fake medicines in Uganda. Social media is awash with the adverse effects of these medicines. So it is true that these medicines are there,” a resident told the writer.
The Pharmacy and Poisons Board has urged Kenyans to take their time and read the front of pack labels of medicines they consume to avoid falling victims.