Since assuming office on September 13, 2022, President William Ruto’s administration has introduced far-reaching changes in the health sector.
The changes are targeted at addressing multiple barriers that hinder access to affordable and quality health care.
They include the collapsing of the 66-year-old National Insurance Fund (NHIF), establishment of six specialised facilities, revamping of Kenya Medical Supplies Agency (KEMSA) and improved infrastructure.
KEMSA has witnessed an increase in fill rate by three per cent from 59 percent in 2022 to 62 per cent in 2024.
This has been achieved through recapitalisation where Sh500 million was disbursed towards increasing drugs and health products.
Other interventions include construction and operationalisation of regional distribution centres in Embakasi, Kisumu and Mombasa.
On Infrastructure, there has been a 1.7 percent increase in level 4 hospitals from 357 in 2022 to 363 in 2024 and six specialised facilities.
To enhance human resource in the ministry, 14 new KMTCs have been opened increasing them from 71 in 2022 to 85 in 2024 with the number of graduates now rising from 15, 915 in 2022 to 22, 695 in 2024.
The transitional process to the new dispensation Social Health Authority (SHA) has already kicked off in earnest and is slated to begin operations on October 1.
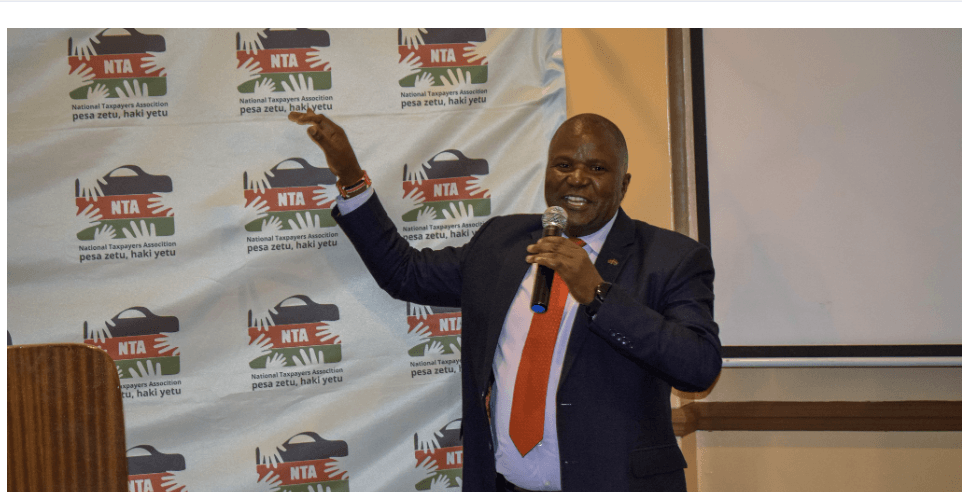
SHA chairman Timothy Olweny says the reforms will not only address gaps that exist under NHIF but will also provide enhanced services to all Kenyans irrespective of their economic status.
The government says the seismic shift in the delivery of health services is critical in the race towards realisation of the Universal Health Coverage (UHC), which has remained unattainable despite past efforts to make it a reality.
The new social health institution was initially meant to begin operations on July 1, 2024, but its implementation was put off due to a number of setbacks.
The registration is on with civil servants directed to enroll into the new health scheme by October 1.
So far about one million Kenyans have registered on the platform while an estimated 10,000 health facilities comprising 2,000 public and 8,000 private and Faith-Based facilities have been licensed to offer services under SHA.
Enactment of new laws
The changes that look set to radically transform the health scene include the enactment of four new laws to provide a legal framework underpinning the new system.
The four laws passed are the Primary Health Care Act, Digital Health Act, Social Health Insurance Act and Facility Improvement Financing Act.
Three funds have also been established, namely the Primary Health Care Fund, Social Health Insurance Fund and the Emergency, Chronic and Critical Illness Fund.
The Kenya Kwanza administration is banking on Primary Health Care to realise the grand project of finally meeting the UHC goal.
The Primary Health Care Fund, which is accessible for free, covers outpatient services at the community facilities classified under primary care networks (PCN).
Public Health Principal Secretary Mary Muthoni says about 150 PCNs have been set up while 41 are in progress.
This is an increase of 2,629 percent as there were only seven in 2022.
The goal is to establish about 315 primary networks across the 47 counties.
One PCN comprises a number of dispensaries, health centres and at least one Level 4 hospital, which is the referral facility for the network.
Unlike the NHIF that assigned Kenyans to one health facility for outpatient services, the SHA will allow patients to access all the lower-level facilities within their PCN.
While primary health care has been in existence for decades, its efficacy has waned over the years due to lack of a clearly defined roles as well as prerequisite laws and regulations.
For instance, Community Health Promoters (CHPs) under SHA, have been in existence for years.
However, they have not been performing their roles optimally, hampered by the absence of an enabling legal and regulatory environment as well as inconsistent payout of their stipend.
Now, Ruto’s administration seeks to turn around this situation and make primary health the centre-piece of its plans to attain UHC.
The prominent features of the new health dispensation are promotion and prevention rather than the current curative system.
Promotion comprises consulting, education and awareness, while prevention focuses on primary, secondary and tertiary screening and immunisation.
At community level, 107,000 Community Health Promoters (CHPs) have been enlisted to champion promotive and preventive care and are paid a monthly stipend of Sh2,500.
This is a 269 percent growth or 78, 000 CHPs.
In 2022, there were only 29, 000 CHPs.
Each of the CHP visits at least 100 households every two to three months.
Bringing healthcare to the doorstep of every Kenyan reduces the need for people to visit hospitals for routine check-ups and screenings.
“Our universal health coverage plan seeks a paradigm shift in the provision of healthcare, from curative to a largely preventive and promotive approach,” said President Ruto during the 60th Jamhuri Day celebrations in Nairobi.
The Emergency, Chronic and Critical Illness Fund has been set up specifically to deal with diseases such as cancer, hypertension and diabetes, which are not only expensive to treat but require long-term management, applying untold pressure on household incomes.
This Fund, resourced by the exchequer like the Primary Health Fund, therefore comes as a huge relief for households.
Upon exhausting the allocation for such chronic diseases under SHIF, households and individuals can access the Chronic Fund for free.
Why SHA?
Under SHA, the government also seeks to make health care provision fair, equitable and progressive.
It seeks to realise this objective through a 2.75 per cent deduction on salaries of formally employed Kenyans.
The amount of contribution by those not in formal employment is determined through a mean testing instrument.
The minimum monthly premium has been slashed from Sh500 to Sh300, a move aimed at reducing the burden of those at the bottom of the pyramid.
More fundamentally, the government will, for the for the first time, pay for all vulnerable Kenyans who are unable to contribute.
Another fundamental NHIF’s shortcoming is its reliance on only salaried Kenyans for premiums, undermining its effort to provide affordable and quality health care for all Kenyans.
To make a clean break from the past littered with inefficiencies,financial mismanagement and fraud that characterised NHIF operations, SHA will operate entirely on a digital ecosystem where only accredited individual doctors and health facilities offer services. The system is also meant to eliminate quacks and illegal clinics.
PS Muthoni noted that shifting to a digital platform is a game-changer in provision of health.
Under SHA, tariffs or charges for illnesses have been standardised, stopping a trend of overcharging by some facilities, a widespread occurrence under NHIF.
If managed effectively, the Social Health Authority has the potential to bring about significant changes in Kenya’s healthcare system.
It promises to reduce financial barriers to healthcare and foster health services for all Kenyans.