In 2019, the government made a strong commitment towards achieving universal health coverage as one of the Big 4 Agenda and started designing and implementing priority reforms to accelerate progress.
The main goal was to refocus on the quality of care and increasing demand for services.
These reforms included increasing the share of (mandatory) pooled resources through a health insurance-based mechanism built on the existing National Health Insurance Fund, enhancing its capacity to function as a strategic purchaser of health services; expanding coverage of health services equitably through an emphasis on primary healthcare and improving public financial management arrangements to enhance the effectiveness of public funds in the devolved health sector.
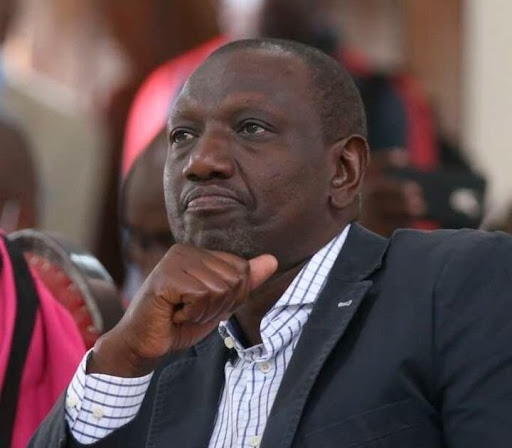
President William Ruto in his manifesto made further commitments to the realisation of the constitutional right to health in the shortest time possible by delivering Universal Health Coverage.
In addition to fast-tracking the ongoing interventions, the new government promised to address the conundrum between healthcare workers’ representatives.
They felt the devolvement of health being managed at the county level was a real short change whereas county governments insist that healthcare workers must be accountable to the county government.
This should be among the first tasks that the new Ministry of Health Cabinet Secretary undertakes after taking the oath to office as it poses a significant risk to the UHC journey.
The manifesto further recognised the 'programmatic engine' for UHC that primary health care presents.
The increased healthcare costs and demand emphasises the need for resource-saving approaches that improve access and maintain a healthy community.
Studies estimate that 70 per cent of cases seen in our hospitals are preventable.
It is approximated that one shilling invested in community health has a return of nine shillings saved in curative health costs.
At the cornerstone of community health that strengthens PHC are the community health workers who carry out functions that are person-centred, support team-based care, address social determinants of health, and promote health care access.
Historically, these frontline health workers have been particularly effective, especially in settings where they share ethnicity, language, socioeconomic status, and life experiences with the communities they serve.
Their response during the Covid-19 outbreak affirmed the same beyond a reasonable doubt.
Currently, county governments are in the process of formulating their County Integrated Development Plans which provide a framework for resource allocation for the next five years.
The county governments ought to maximise the untapped potential of investing in community health workers by allocating programs and budgets to strengthen their structures, knowledge, and stipend.
Integrating trained, motivated and effective CHWs working at a scale as part of an integrated health system will deliver multiple benefits and expedite progress toward realising UHC and improving the overall efficiency and sustainability of health systems within the larger efforts to strengthen health systems.
Youth coordinator at the Centre for the study of adolescence
Edited by Kiilu Damaris