The growth of palliative medicine has been phenomenal in Kenya starting in the 1990s when the first hospice was set up. Palliative care providing units, be they hospices or hospital-based, have now topped 45, thanks to the countrywide training by the Kenya Hospices and Palliative Care Association in partnership with other stakeholders.
According to the Centre to Advance Palliative Care, the specialty is fast growing in the field of medicine worldwide and has many young doctors interested in pursuing the profession.
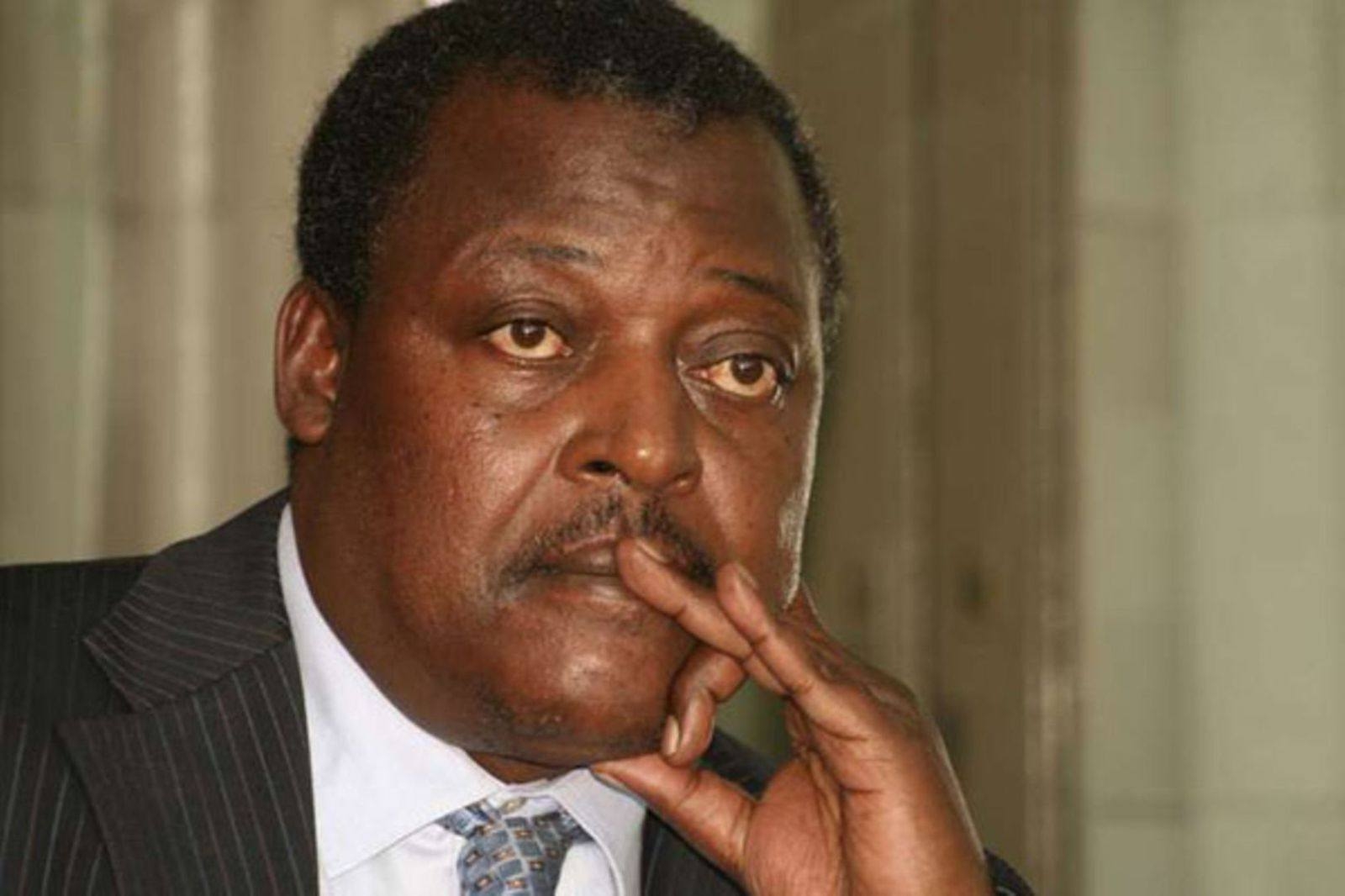
Through much advocacy and petition to the ministry of health and the Medical Practitioners and Dentists Board, Palliative Medicine was gazetted as a medical specialty in 2012. This has culminated in the declaration of the first palliative medicine specialist in the country, Dr John Weru, who is also the leader of the palliative care team at the Aga Khan University Hospital.
His interest in this field started immediately after completing undergraduate studies and picked as he learned more about palliative care on his own as there were no other doctors trained in the field to guide or teach him. He then set out to undertake post graduate studies in this specialty which has seen him study in Oxford Brookes University, University of Dundee, both in the UK, and the Institute of Palliative Medicine at San Diego in California, USA.
“I grew more excited about palliative medicine and came to realise that it is something I would find rewarding and enjoyable if I got good at it over time. I found more satisfaction in palliative care encounters with patients and became less comfortable with what I perceived as occasional lack of holistic patient care," says Dr Weru
According to the doctor, palliative care is a medical specialty that focuses on comfort, relief of symptoms, and clarifying patient’s treatment goals. It can be offered concurrently with other medical therapies for any seriously ill patient with any disease or condition, particularly when there are physical, psycho-social, or spiritual complications. The main aim is to treat the patient’s symptoms, provide supportive care while understanding the patient’s aspirations and goals.
It also ensures that patients and their families are fully informed of the diagnosis and the likely outcomes in a timely, sensitive and appropriate manner. It is about treating the patient’s pain, fatigue, nausea and vomiting, weight loss, loss of appetite, difficulty in breathing and many others. For example, a patient diagnosed with cancer will suffer many of these symptoms and timely assessment and treatment reduces the distress these patients and their families suffer from.
Patients and families who have experienced palliative care say that it maximizes quality of life and empowers patients and their families to make treatment decisions more in line with their hopes and values. Palliative care gives an emotional lift to providers, while reducing hospital expenses. It is also considered as an additional tool for enhancing care transitions, thus reducing hospital stay and readmission rates.
Dr Weru further notes that palliative care is an incredibly intense service but richly rewarding. “It allows us to give care to people living at the most vulnerable times of their lives. Just like in any other medical discipline, some core elements of palliative care such as aligning the patient’s treatment with their goals and basic symptom management should be routine aspects of care delivered by any doctor. Other skills are more complex and take years of training to learn and apply, such can include negotiating a difficult family meeting, addressing existential distress, addressing ethical-legal challenges facing patients and their families and also doctors treating these patients. This is coupled with managing refractory symptoms such as severe pain, severe fatigue and require palliative medicine specialists to do so”.
“Many hospitals have now realised the importance of these services to their clients. At the Aga Khan University Hospital, palliative care services are fully accredited and offer both inpatient and outpatient care to patients in the hospital and those who are referred from other health facilities. The service has now been in existence for the last one year and there has been positive feedback from patients and their families regarding the quality of care being provided.”
“The duty now for palliative medicine specialists is to teach other doctors and clinicians as this is a very new medical specialty practice in the country, to set up structures and processes for the growth and development of the service and to provide the much needed clinical care to patients and their families.”