The Mpox outbreak in May 2024 caused alarm in Eastern and Southern Africa with the World Health Organisation declaring it an emergency three months later in August.
Kenya would record its first case of the viral disease barely two weeks after the WHO alarm sparking widespread fear.
Would the disease bring the country and the region to a standstill again necessitating shutdown akin to the Covid-19 pandemic?
Mpox is an infectious disease that causes painful rash, enlarged lymph nodes and fever.
Patients often recover although the disease can be deadly.
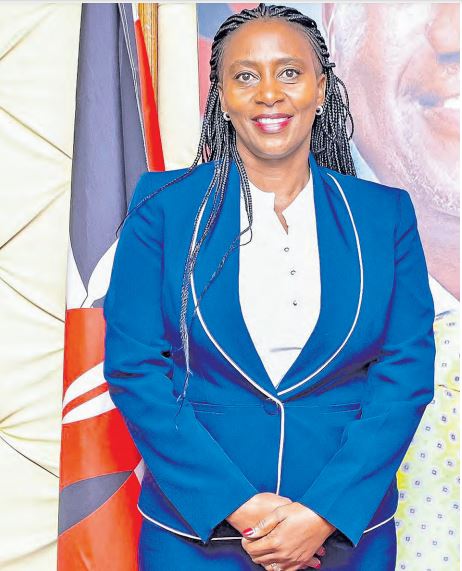
But as the saying goes, cometh the hour, cometh the man and so did Principal Secretary Mary Muthoni emerge.
The Public Health and Professional Standards PS quickly unveiled strategies to contain the disease by enhancing surveillance for early detection and activating a robust laboratory network for rapid diagnosis and effective isolation of cases.
Those efforts coupled with an activated emergency response system and timely training for healthcare workers to identify and manage the disease has contained the virus to just 28 cases across 12 counties by the second week of December.
It is PS Muthoni’s steady hand in containing and managing the Mpox outbreak and role in promoting Universal Health Coverage that Kenyans saw befitting for her nomination as the Star Person of the Year.
The PS spoke to AGATHA NGOTHO.
Q: What were the challenges in managing the Mpox crisis?
One major challenge was combating misinformation about Mpox, which created panic and stigma. We addressed this through public sensitisation campaigns and transparent communication and community engagements. We also had challenges in ensuring adequate testing and reporting in remote areas. We decentralised laboratory services and worked with counties to streamline data collection and case management.
Q: How important were public awareness campaigns in the fight against Mpox?
Public sensitisation remains critical in containing the spread of Mpox. We conducted targeted campaigns using local languages, radio and community health promoters to share prevention measures. Highrisk populations, such as healthcare workers and vulnerable groups were prioritised for education on symptoms, prevention and reporting suspected cases.
Q: What key lessons has Kenya learned from the Mpox outbreak?
Key lessons include the importance of robust surveillance systems, community involvement, and multi-sectoral collaboration. We also learned that timely and clear communication can prevent misinformation and panic. Moving forward, Kenya will continue to invest in preparedness and ensuring health systems are agile enough to respond to emerging threats. On Championing Universal Health Coverage
Q: UHC is a core goal for the ministry. What are the major milestones Kenya has achieved so far?
We have made significant progress with the rollout of Social Health Insurance under the Social Health Authority. Key achievements include the deployment of Community Health Promoters to deliver healthcare at the grassroots level, the revival of the Linda Mama programme to improve maternal care and the Health Facility Census that identified infrastructural gaps within our facilities. These have informed targeted investments in healthcare infrastructure.
Q: How do you ensure equity and inclusivity in UHC policies, particularly for vulnerable and underserved populations?
Equity is central to our approach; the goal of Universal Health Coverage is to ensure Kenyans from all walks of life have access to affordable and quality health services. We focus on ensuring that the vulnerable, including women, children, and persons in low-income areas, can access healthcare without financial hardships. Through SHIF, subsidies are provided for vulnerable households, ensuring no one is left behind.
Q: What role do NGOs and the private sector play in UHC?
Partnerships are instrumental. International organisations like WHO and Global Fund provide technical and financial support, while NGOs enhance service delivery by working with the ministry in various programmes at community levels, especially in remote areas. The private sector contributes through innovation, infrastructure development, and investment in medical supplies. Collaboration ensures a more resilient and inclusive healthcare system.
Q: UHC is long-term. How is Kenya planning to ensure sustainable financing for the health sector, especially in the face of economic challenges?
Sustainable financing is critical. We are enhancing domestic resource mobilisation through government funding, strengthening public-private partnerships, and exploring innovative financing models. Additionally, through integrating health insurance contributions and ensuring efficient use of available resources, we aim to secure longterm financial sustainability.
Q: Sanitation is a key aspect of public health. What initiatives has the ministry put in place to improve sanitation standards across the country?
The ministry has established a robust enabling environment through policy formulation e.g Costed Kenya rural sanitation and hygiene roadmap 2023/2030 which guides national and county governments as well as development partners in implementation of sanitation policies. The roadmap sets objectives to be achieved for the sector by 2030. They include the adoption of sanitation marketing and market activation activities to address supply of sanitation solutions. We also launched Epuka Uchafu Afya Nyumbani initiative to sensitise communities to take responsibility in keeping their environment clean and healthy. The ministry also established Kenya Sanitation Alliance, a movement which convenes on quarterly basis with the main focus of eradicating open defecation in some 15 high burden counties to improve public health.
Q: How do you engage communities in improving sanitation?
House to house campaigns through community led total sanitation approach and while working with community health promoters. Clean up campaigns through both public and institutional structures, mobilisation of domestic resources through Kenya Sanitation Alliance, and conducting annual sanitation week during the third week of November where communities are engaged in clean up exercises.
Q: As the PS in charge of Public Health, how do you view your leadership role in transforming healthcare in Kenya?
My role is to provide strategic leadership and ensure policies are people-centered, evidence-based, and impactful. I strive to inspire collaboration, strengthen systems, and champion health equity to revive the face of public Health in Kenya and achieve our national goals.
Q: Looking ahead, what are the top public health priorities that need urgent attention?
Key priorities include tackling emerging diseases, improving maternal and child health, and addressing non-communicable diseases. We will focus on preventive health, strengthen healthcare systems, and scale up digital health solutions for better access and efficiency.
Q: What drives your passion for public health and service?
Public health impacts everyone. My passion comes from knowing that preventive health measures save lives and improve communities. Seeing positive outcomes, particularly for the underserved, motivates me to do more.
Q: What is your advice for the next generation of public health leaders in Kenya?
Be innovative, resilient, and committed to evidence-based policies. Prioritiae equity and listen to the voices of the communities you serve. Collaboration and adaptability will be your greatest strengths.
Q: What is your parting shot?
Health is not just a service, it is a
human right. Let’s work together
to strengthen health systems, promote prevention and achieve UHC
for all. I urge all Kenyans to register
for the transformative Social Health
Authority through *147# www.SHA.
go.ke. A healthier Kenya is a more
productive and prosperous Kenya.