
The amount was from 937 cases filed by officers within the service out of the total 1,756 submitted.
There are 161 cases which are currently being processed amounting to Sh108 million while 240 others under the Group Personal Accident (GPA) cover amounting to Sh289 million was rejected.
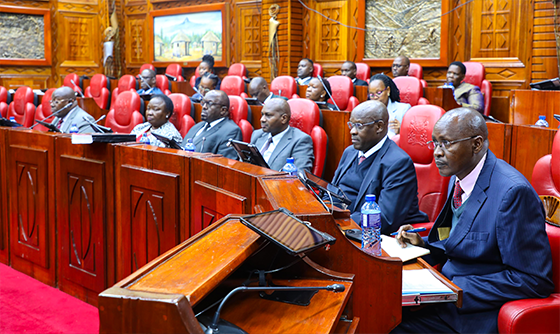
In a document tabled before the Senate by NPSC CEO Peter Leley, other outstanding claims remain due to various reasons.
They include 116 cases, totaling Sh110 million, pending due to documentation issues, and 422 cases, amounting to Sh444 million, under internal review by the Social Health Authority (SHA), formerly NHIF.
Additionally, 65 claims submitted beyond the 24-month deadline total Sh81 million, while 63 cases, worth Sh69 million, are awaiting execution of discharge vouchers.
Furthermore, 158 disputed claims, amounting to Sh264 million, are pending waiting for a second review.
Leley was appearing before the Committee on National Security, Defence and Foreign Relations to respond to a petition concerning compensation of police officers injured in the line of duty.
He was accompanied by commission chairperson Eliud Kinuthi among other commissioners. It was filed by six police officers.
Compensation to the members of the disciplined service is made in line with the Work Injury Benefits Act (WIBA), 2007.
The Act provides for compensation to employees for work-related injuries and diseases contracted in the course of their employment.
The state department of Interior entered into a deal with the defunct National Hospital Insurance Fund (NHIF) to provide the group life cover, work injury Benefits Act (WIBA) and GPA for the members of the National police service.
Compensation is provided in form of salary continuation or a lump sum based on the officer’s annual gross salary.
For permanent disability as a result of illness, an officer is paid a one-year basic salary multiplied by the percentage awarded.
In the case of death, illness, or injury as a result of occupation injuries, an officer is entitled to eight years gross salary.

Kinuthia was quick to absolve the commission from any blame for the delay in the release of the dues instead pointing an accusing finger at NHIF.
He wondered why NHIF has continued to subject the injured officers to a second medical review even after the Director of Occupational Safety and Health Services (DOSH) had okayed it.
The Kenya Police Service accounted for the highest number of claims of 998 while Administration Police had 686.
Those from the Directorate of Criminal Investigations had 72 claims during the period.
“The obligation to make payments within 90 days as stipulated in section 26 94) of Work Injury Benefits Act (WIBA) rests with the service provider (NHIF), but in most cases, these timelines were not adhered to despite the National police service’ timely remittance of premiums and submissions of claims,” he said.
He pointed out that NHIF has failed to meet its obligation under the contract to settle the assessed claims within 90 days.
Kinuthia further expressed concern over the exemption of NHIF from regulation by the Insurance Regulatory Authority (IRA) saying it has left the National Police Service exposed to mismanagement by NHIF.
The then Treasury Cabinet Secretary Ukur Yatani exempted the insurer in a Gazette Notice dated April 17, 2020.

Procedure for making a claim
The procedure for processing an injury claim begins with the affected officer reporting about the accident to the immediate commander.
The commander then submits a formal notification commonly referred to as a signal to police headquarters with the necessary details about the incident.
A claim processing officer then fills Form 1 at the Directorate of Occupational Safety and Health Services.
Once the officer has recovered from injury or during recovery, they are required to avail a medical report, identification documents, bank account details, and police abstract.
In the unfortunate case of death, a death certificate, burial permit, and a postmortem report are required.
After gathering all necessary documents, the claim is compiled by the claims office and submitted to the Insurance Service Provider with an official forwarding letter.
Upon receipt of the claim, the Insurance provider forwards it to DOSH for further action.
The DOSH then schedules a medical assessment for the injured officer to determine the degree of disability caused by the accident.
Following the assessment, the DOSH prepares an agreement form that outlines the computed amount for compensation.
The injured officer or the next of kin, in case of death, is then called upon to review the computed amount and sign the agreement to confirm acceptance of the compensation amount.
Once the agreement is signed, the claim is then submitted to the insurer or other designated service Provider from the actual payment of compensation.












