
A study found two versions of moxifloxacin were more palatable than generic alternatives on the market.
The research is part of the ChilPref ML study, an initiative led by Stellenbosch University in South Africa in collaboration with the TB Alliance and funded by Unitaid.
Anthony Garcia-Prats, one of the study authors and an associate professor at the University of Wisconsin in Madison, said scientists have made strides in developing new treatments for drug-resistant TB.
It was previously one of the most difficult diseases to manage and there were few child-friendly options.
“Now we are making sure these medicines are appropriate for children, starting with taste, which is an aspect children and parents say is critical,” Garcia-Prats said.
Moxifloxacin, however, is one of four drugs in the new four-drug all-oral BPaLM treatment for multidrug-resistant tuberculosis. It consists of bedaquiline, pretomanid, linezolid and moxifloxacin.
This treatment is given when TB is either resistant to rifampicin, a critical first-line drug, or rifampicin and isoniazid, another first-line drug combination. These resistant strains are collectively referred to as RR/MDR-TB.
An estimated 25,000 to 32,000 new cases of RR/MDR-TB among children 14 years of age and younger are recorded annually, the study indicates.
“This population is extremely sensitive to the taste of medicine. Although young children are not yet recommended to receive this regimen, children still frequently receive moxifloxacin in other regimens,” the study reads.
Graeme Hoddinott, the principal investigator of the study, said it takes six to nine months to treat a case of RR/MDR-TB. That is a long time for parents to struggle with getting their children to take bitter-tasting medicine.
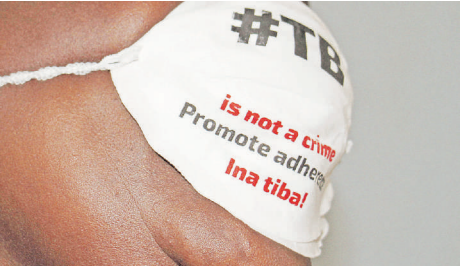
“We cannot treat children in a humane manner for drug-resistant TB if the medicines taste so terrible that children refuse them or must be forced to take them,” Hoddinott from Stellenbosch University said.
Moxifloxacin may also increasingly be used in the future for the treatment of drug-susceptible TB, which affects an estimated 1.2 million children globally each year.
“Ensuring children have access to effective and palatable TB treatments is a crucial step in improving adherence and treatment outcomes,” Koteswara Rao Inabathina, one of the study’s authors and CMC (Carboxymethyl cellulose) project manager at TB Alliance, said.
“Through close collaboration with manufacturers, we have addressed critical unmet needs by developing practical solutions that make available and effective drug-resistant TB treatments not only accessible but also palatable and acceptable for children.”
The study showed the approach was safe, feasible, inexpensive and could be readily replicated for other existing and new drugs for TB and other diseases. It demonstrated it is possible to engage with children to identify their taste preferences for the medicines they will be taking.
“The easier we can make it for a child to take their medicines regularly, the more likely it is they will complete their treatment successfully,” Unitaid senior technical manager Cherise Scott said.
“We will not allow children to be neglected in global health responses simply because their needs are more complex.”












